|
 |
YOUNG DIABETES RESEARCH –YDR PROJECTS
|
|
|
Currently YDR projects is supervised by Dr.A.Amutha. Research activities include research areas of basic, epidemiological, clinical and bio chemical profile and complications of type 1 diabetes and type 2 diabetes especially in young, children and adolescents. The team was involved in studying the pathophysiology of type 2 diabetes especially the role of beta cell function and insulin sensitivity among young individuals. Currently, involved in nationwide Registry of diabetes in India at young at onset (ICMR) and harmonization of registries from US (SEARCH) and India(YDR).
|
|
| |
|
|
| |
Vision |
|
| |
To study the clinical profile of diabetes in the children, adolescents and young adults and its various complications. |
|
| |
|
|
| |
Mission |
|
| |
To identify the risk factors for complications and to find out the impact of various strategies (by Yoga, Fitness and Zumba) to prevent complications in young type 1 and type 2 diabetes. |
|
| |
|
|
| |
PROJECTS UNDERTAKEN AND ONGOING |
|
| |
|
|
| |
1. ICMR - REGISTRY OF PEOPLE WITH DIABETES IN INDIA WITH YOUNG AGE AT ONSET - Phase I (2006 -2012) & Phase II (2012 -2020)
5/3/2/registry/diab/04-NCD-II (ONGOING)
The protocol of ICMR’s Task Force project on “Registry of People with Diabetes with Young Age at the Onset” was implemented through the three different units during phase II viz: Coordinating Units, ICMR Regional Collaborating Centres and Collaborating Centres. The ICMR Regional Collaborating Centres are the participating centres in phase I (initiated in 2006) and collect data on voluntary basis from Reporting Centres. These Centres would be assigned the responsibility of monitoring collaborating centres region wise. Our research team was one of the ICMR Regional Collaborating Centre.
Primary objective of the project was:
To understand:
- the magnitude of problem
- disease pattern or types including the geographic variation
- incidence and prevalence rate of complications
Secondary objective:
The registry is aimed
- Facilitate research in the areas of basic, clinical (including patterns of care and survival), epidemiological, genetic and molecular levels.
- Help promoting awareness about the magnitude of problem among professionals, public health partners.
- Help in Diabetes Monitoring Programme.
- Assist in the development of management guidelines.
- Develop human resources in diabetes epidemiology.
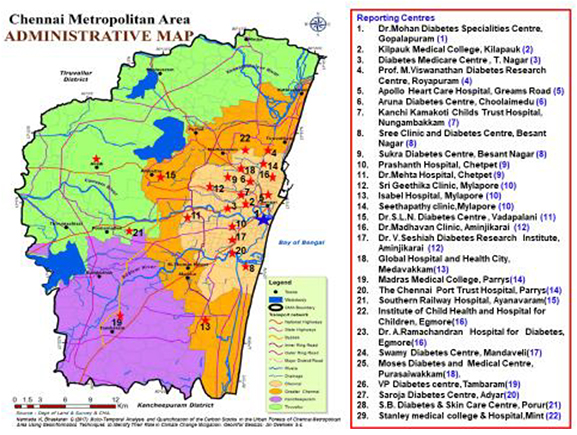
Being one of the Collaborating Centres, the team approached all the hospitals and clinics in Chennai to participate in this registry. So far 29 Reporting centres participates in this ICMR young diabetes registry and in Phase 1, 1784 data were collected from these reporting centres. The data collected were on demographic, personal information, clinical, anthropometric, biochemical values, diabetes type, complication, mode of treatment, etc. being collected through the questionnaire approach. The information on follow up would be collected in a separate follow up proforma. The following figure shows the Reporting centres from Chennai who were involved in the registry. |
|
| |
 |
|
| |
|
|
| |
2. Beta cell function in youth with type 2 diabetes and itsAssociation with atherosclerosis
DST No: SR/SO/HS-0135/2009 (COMPLETED)
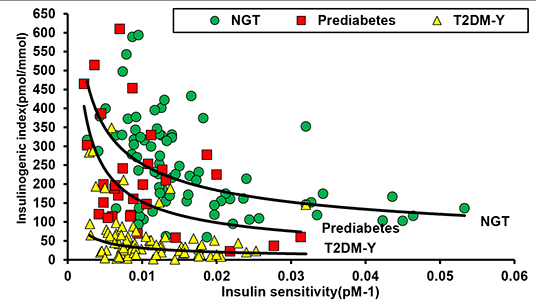
This project was conducted with the following objectives: to assess the independent associations of beta cell dysfunction and insulin resistance (IR) with T2DM-Y and to describe the prevalence of, and risk factors for, early atherosclerosis in T2DM-Y. The study enrolled type 2 diabetes in youth (T2DM-Y) cases (n=82), were age and sex matched Controls, individuals with normal glucose tolerance (n=31) and Youth with prediabetes (IFG and IGT) (n=83).
Observations from the study were:
- Subjects with prediabetes had a more drastic decline in DIo than an increase in HOMA-IR when compared to normal glucose tolerant subjects, suggesting an early and significant change in the β-cell dysfunction disrupting glucose metabolism. These points to a predominant role played by β-cell dysfunction in the pathogenesis of prediabetes and T2DM-Y in our population who are relatively lean compared to Europeans.
- DIo derived by OGTT measurements were 9-fold lower in our T2DM-Y when compared to NGT.
- When compared to other risk factors like BMI, Waist and insulin resistance, β-cell dysfunction occurring early in the natural history may be a key factor in pathogenesis of T2DM in Asian Indians.
- A simple surrogate OGTT protocol could provide estimates of insulin sensitivity and β-cell function which could be detected in high risk youth at an early stage. It can also be used in large-scale epidemiological studies where the use of doing clamp studies is not feasible.
- The non-linear relationship between sensitivity and secretion is best described by a hyperbola. The hyperbolic relationship means that the product of insulin sensitivity and insulin secretion is constant for a given degree of glucose tolerance, and the final outcome of the above is called the disposition index (DIo). Since we have both the insulin measures we can find out the hyperbolic relationship for the NGT, prediabetes and T2DM-Y groups as given below.
|
|
| |
 |
|
| |
|
|
| |
3. Harmonization of existing registries of diabetes in youth: a U.S.-India Collaborative Research Partnership
R21 DK105869-01(ONGOING)
This project aims to compare the epidemiologic characteristics of diabetes in youth between India and the U.S. Knowledge of prevalence, incidence, mortality, and clinical presentation, treatment, quality of care and quality of life differ between countries and this will bring new insights into the potential causes and improved treatment. A sensitive surveillance system in both countries can also inform policy about whether changes in underlying risk factors such as obesity, environmental exposures and other factors are leading to an increase in risk, or whether improved nutrition and environmental hygiene have reduced risk over time.
The specific aims of this proposal are to 1. To harmonize the Indian YDR and the SEARCH registry in the U.S. Clinical YDR and SEARCH data in sufficient areas to be useful for initial comparisons; 2. To compare phenotypic, clinical and demographic characteristics by type of diabetes between YDR and SEARCH. This will improve our understanding of clinical presentation, treatment patterns and evolution of diabetes in youth, according to diabetes type, in the 2 countries. 3. To compare the burden of diabetes in youth by age, sex, race/ethnicity and type of diabetes between India and the US. A minimum dataset will be developed and harmonized which will allow the prevalence of diabetes in youth and young adults to be compared between countries, by type of diabetes and other demographic factors. This project will likely include only selected Indian YDR sites, but all SEARCH sites. |
|
| |
|
|
| |
Publications: |
|
| |
- Sai Prasanna N, Amutha A, Pramodkumar TA, Anjana RM, Venkatesan U, Priya M, Pradeepa R, Mohan V. The 1 h post glucose value best predicts future dysglycemia among normal glucose tolerance subjects. Journal of Diabetes and Its Complications. 2017 2Nov;31(11):1592-1596. doi: 0.1016/j.jdiacomp.2017.07.017.
- Amutha A, Pradeepa R, Chella KS, Anjana RM, Unnikrishnan R, Mohan V. Lipid Profile in Childhood-and Youth-Onset Type 2 Diabetes and their Association with Microvascular Complications. Journal of Association of Physicians of India. 2017;65:42-47.
- Unnikrishnan R, Anjana RM, Amutha A, Ranjani H, Jebarani S, Ali MK, Narayan KMV, Mohan V. Younger- onset versus older-onset type 2 diabetes: Clinical profile and complications. Journal of Diabetes and Its Complications. 2017; 31:971 – 975.
- Reddy S, Amutha A, Rajalakshmi R, Bhaskaran R, Monickaraj F, Rangasamy S,Anjana RM, Abhijit S, Gokulakrishnan K, Das A, Mohan V, Balasubramanyam M.Association of increased levels of MCP-1 and cathepsin-D in young onset type 2 diabetes patients (T2DM-Y) with severity of diabetic retinopathy. J Diabetes Complications. 2017 Mar 10. pii: S1056-8727(16)30839-X.
- Amutha A, Unnikrishnan R, Anjana RM, Mohan V. Prepubertal Childhood Onset Type 2 Diabetes Mellitus: Four Case Reports. JAPI. 2017;65;43-46.
- Amutha A, Anjana RM, Venkatesan U, Ranjani H, Unnikrishnan R, Narayan KMV, Mohan V, Ali MK, Incidence of complications in young-onset diabetes: Comparing type 2 with type 1 (The young diab study), Diabetes Research and Clinical Practice. 2017; 213 : 1 - 8.
- Shruti S, Mohan V, Amutha A, Aravindhan V. Increased serum levels of novel T cell cytokines IL-33, IL-9 and IL-17 in subjects with type-1 diabetes. Cytokine. 2016; 86; 6-9. http://dx.doi.org/10.1016/j.cyto.2016.07.007.
- Anand K, Vidyasagar S, Lasrado I, Pandey GK, Amutha A, Ranjani H, Mohan Anjana R, Mohan V, Gokulakrishnan K. Secreted Frizzled-Related Protein 4 (SFRP4): A Novel Biomarker of β-Cell Dysfunction and Insulin Resistance in Individuals With Prediabetes and Type 2 Diabetes. Diabetes Care. 2016 Jul 6.pii: dc160756.
- Amutha A, Mohan V. Diabetes Complications in Childhood and Adolescent Onset Type 2 Diabetes – A Review. J Diabetes Complications. 2016. Feb 9. pii: S1056-8727(16)00060-X. doi: 10.1016/j.jdiacomp.2016.02.009.
- Priya M, Amutha A, Pramodkumar TA, Ranjani H, Jebarani S, Gokulakrishnan K, Pradeepa R, Unnikrishnan R, Anjana RM, Mohan V. Both βeta cell function and insulin sensitivity in normal glucose tolerant subjects stratified by 1-hour plasma glucose values. Diabetes Technol Ther. 2016 Jan;18(1):29-33.
- Anjana RM, Amutha A, Mohan V. Regularity of follow-up, glycemic burden, and risk of microvascular complications in patients with type 2 diabetes: a 9-year follow-up study: Reply to Dr. Tasci et al. Acta Diabetol. 2016 Feb;53(1):131-2.
- Gokulakrishnan K, Amutha A, Ranjani H, Subramanian Y Bibin, Balakumar M, Gautam Kumar P, Anjana RM, Ali MK, Venkat Narayan KM, Mohan V. Relationship of adipokines And Proinflammatory Cytokines Among Asian Indians With Obesity And Youth Onset Type2 Diabetes. Endocr Pract. 2015 Oct;21(10):1143-51.
- Amutha A, Ali MK, Unnikrishnan R, Anjana RM, Ranjani H, Gokulakrishnan K,Mohan V, Narayan KM. Insulin sensitivity and secretion in youth onset type 2 diabetes with and without visceral adiposity. Diabetes Res Clin Pract. 2015 Jul;109(1):32-9.
- Gokulakrishnan K, Manokaran K, Pandey GK, Amutha A, Ranjani H, Anjana RM,Mohan V. Relationship of betatrophin with youth onset type 2 diabetes among Asian Indians. Diabetes Res Clin Pract. 2015 Jul;109(1):71-6.
- Billow A, Anjana RM, Ngai M, Amutha A, Pradeepa R, Jebarani S, Unnikrishnan R,Michael E, Mohan V. Prevalence and clinical profile of metabolic syndrome among type 1 diabetes mellitus patients in southern India. J Diabetes Complications. 2015;29(5):659-64.
- Kanthimathi S, Chidambaram M, Liju S, Bhavadharini B, Bodhini D, Prakash VG, Amutha A, Bhavatharini A, Anjana RM, Mohan V, Radha V. Identification of Genetic Variants of Gestational Diabetes in South Indians. Diabetes Technol Ther. 2015 Jul;17(7):462-7.
- Anjana RM, Shanthirani CS, Unnikrishnan R, Mugilan P, Amutha A, Nair HD, Subhashini S, Venkatesan U, Ali MK, Ranjani H, Mohan V. Regularity of follow-up, glycemic burden, and risk of microvascular complications in patients with type 2 diabetes: a 9-year follow-up study. Acta Diabetol. 2015 ; 52(3):601-9.
- Vendhan R, Amutha A, Anjana RM, Unnikrishnan R, Mohan V. Clinical Profile of Non Alcoholic Fatty Liver Disease Among Young Patients with Type 1 Diabetes Mellitus Seen at a Diabetes Speciality Centre in India. Endocr Pract. 2014;20(12):1249-57.
- Rajalakshmi R, Amutha A, Ranjani H, Ali MK., Unnikrishnan R, Anjana RM, VenkatNarayan KM, Mohan V. Prevalence and risk factors for diabetic retinopathy in Asian Indians with young onset type 1 and type 2 diabetes. J Diabetes Complications 2014.May-Jun;28(3):291-7.
- Vendhan R, Amutha A, Anjana RM, Ranjit Unnikrishnan, Deepa M, Mohan V. Comparison of characteristics between non obese and overweight/obese subjects with non alcoholic fatty liver disease in a south Indian population. Diabetes Technology and Therapeutics. 2014 Jan;16(1):48-55.
- Amutha A, Thai K, Mohan V. Childhood and Adolescent Onset Type 1 Diabetes in India. MGM J Med Sci 2013;1(1):46-53.
- Gokulakrishnan K, Aravindhan V, Amutha A, Shiny A, Ranjani H, Anjana R M, Ranjit Unnikrishnan, Priya Miranda, Venkat Narayan KM, Mohan V. Serum adiponectin helps to differentiate type 1 and type 2 diabetes among young Asian Indians. Diabetes Technology and Therapeutics. 2013 Aug; 15(8):696-702.
- Mohan V, Rani CS, Amutha A, Dhulipala S, Anjana RM, Parthasarathy B, Unnikrishnan R. Clinical Profile of Long-Term Survivors and Nonsurvivors With Type 2 Diabetes. Diabetes Care. 2013. Aug; 36(8):2190-7.
- Mohan V, Amutha A, Ranjani H, Unnikrishnan R, Datta M, Anjana RM, Staimez L, Ali MK, Narayan KMV. Associations of b-Cell Function and Insulin Resistance with Youth-Onset Type 2 Diabetes and Prediabetes Among Asian Indians. Diabetes Technology and Therapeutics. 2013; 15:315-322.
-
Jahnavi S, Poovazhagi V, Mohan V, Bodhini D, Raghupathy P, Amutha A, Kumar PS, Adhikari P, Shriraam M, Tanvir K, Das A, Molnes J, Njolstad P, Unnikrishnan R, Radha V; Clinical Molecular characterization of Neonatal diabetes monogenic syndromic diabetes in Asian Indian Children. Clinical and molecular characterization of neonatal diabetes and monogenic syndromic diabetes in Asian Indian children. Clin Genet. 2012;Jul 25;9999(9999).
- Venkataraman V, Amutha A, Anbalagan VP, Deepa M, Anjana RM, Unnikrishnan R, Vamsi M, Mohan V. Association of glycated hemoglobin with carotid intimal medial thickness in Asian indians with normal glucose tolerance. Journal of Diabetes and its complications. 2012; 26: 526-530.
- Amutha A, Manjula Datta, Ranjit Unnikrishnan, Anjana RM, Mohan V. Clinical Profile And Complications Of Childhood And Adolescent Onset Type 2 Diabetes Seen at a Diabetes Centre in South India. Diabetes Technol Ther. 2012 Jun; 14(6):497-504.
- Amutha A, Manjula Datta, Mohan V. Type 2 Diabetes in Children – An Emerging Problem in India. Indian Journal of Practical Pediatrics. 2011; 13(4) 409- 416.
- Amutha A, Datta M, Unnikrishnan IR, Anjana RM, Rema M, Venkat Narayan KM, Mohan V. Clinical profile of diabetes in the young seen between 1992 and 2009 at a specialist diabetes centre in south India. Prim Care Diabetes. 2011 Dec; 5(4):223-9.
- Mohan V, Ravikumar R, Poongothai S, Amutha A, Sowmya S, Karkhuzali K, Parkin CG. A single-center, open, comparative study of the effect of using self-monitoring of blood glucose to guide therapy on preclinical atherosclerotic markers in type 2 diabetic subjects. J Diabetes Sci Technol. 2010 Jul 1;4(4):942-8
- Mohan V, Pranjali PP, Amutha A, Ganesan A, Manjula Datta, Gayathri P. Prevalence And Clinical Profile Of Autosomal Dominant Type 2 Diabetes In Asian Indians. Primary Care Diabetes 3 (2009) 233-238
|
|
| |
|
|
| |
Research Team |
|
| |
 |
Dr. A. Amutha
Mrs. P. Latha
Mrs. V. Shanthalakshmi
|
Scientist
Research Assistant
Data Entry Operator |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
 |
|
|
| |
|
|